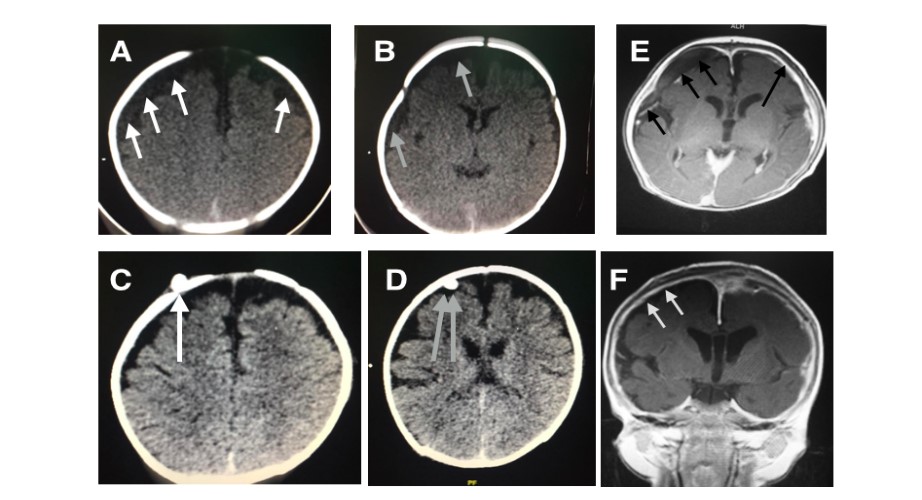
Cryptogenic subdural empyema mimicking subacute-subdural hematoma on CT imaging in the pediatric group: a clinical case series
DOI:
https://doi.org/10.46900/apn.v5i1.166Keywords:
Escherichia Coli, Subdural hematoma, Infant, antibiotic therapy, Empyema, Acquired, Community, Infection, Subdural empyema (SDE), GCS, SeizureAbstract
Introduction: Subdural empyema (SDE) is a rare but potentially life-threatening intracranial infection that is invariably fatal if left untreated. As clinical and radiologic features may be subtle or uncertain, early diagnosis may be a challenge but is crucial in reducing morbidity and mortality. SDE should always be suspected especially in a paediatric group with a history of fever, focal seizures, meningism and neurological deficit. The management of SDE has been debated in the literature for decades. Being one of the most serious neurosurgical emergencies, goals include surgical evacuation where both burr-hole drainage and craniotomy are primary surgical options, treatment of pus, and establishing the etiologic agent which subsequently guides antibiotic therapy for a favourable outcome.
Case presentation: We present three cases of immunocompetent patients, 4 and 6-month-old infants with a 14-year-old adolescent presenting with SDE without underlying risk factors. Non-contrast computed tomography imaging was equivocal for SDE. All of them required surgery. The two infants underwent burr holes and subsequently a wide craniotomy with intravenous antibiotics therapy while the adolescent required craniectomy because of swollen brain. They all had a favourable outcome on long term follow up.
Conclusion: Paediatric supratentorial SDE, although rapidly fatal if not identified promptly, can be effectively managed with early surgical drainage preferably craniotomy, eradication of the source, and sensitive IV broad-spectrum antibiotics. In this article, we discuss the clinical presentation, diagnostic tools, treatment options and outcomes for SDE with an emphasis on the challenges.
Downloads
Additional Files
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Mohammad Jaweed, Dollicia Toh Ching Ying, Esther Sim Wan Rong, Mohammad Ajmal Yasin, Azmin Kass bin Rosman

This work is licensed under a Creative Commons Attribution 4.0 International License.

When publishing in Archives of Pediatric Neurosurgery journal, authors retain the copyright of their article and agree to license their work using a Creative Commons Attribution 4.0 International Public License (CC BY 4.0), thereby accepting the terms and conditions of this license (https://creativecommons.org/licenses/by/4.0/legalcode).
The CC BY 4.0 license terms applies to both readers and the publisher and allows them to: share (copy and redistribute in any medium or format) and adapt (remix, transform, and build upon) the article for any purpose, even commercially, provided that appropriate credit is given to the authors and the journal in which the article was published.
Authors grant Archives of Pediatric Neurosurgery the right to first publish the article and identify itself as the original publisher. Under the terms of the CC BY 4.0 license, authors allow the journal to distribute the article in third party databases, as long as its original authors and citation details are identified.